How to create SMART weight loss goals and achieve them?
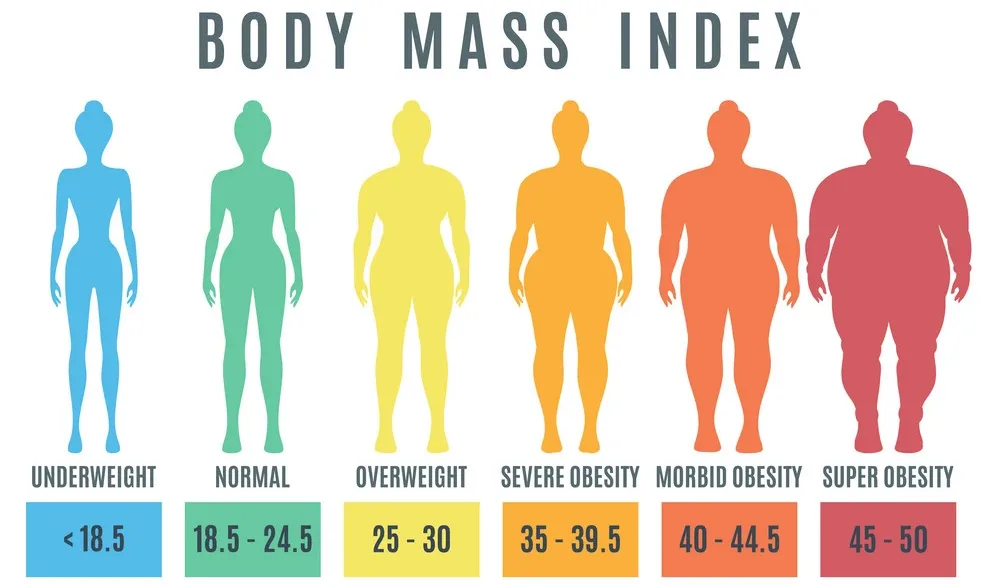
Houston Endocrine Center2022-12-07T13:29:48+00:00Setting and achieving weight loss goals is important, but it can be tricky. It’s not just about eating less and exercising more—it’s also about creating goals that are specific, measurable, actionable, realistic, and timely (SMART). In this article, we will discuss, How to create SMART weight loss goals and achieve them

Why Are Goals Important?
Setting SMART weight loss goals can help keep you motivated. When you set a goal, it gives you something to work towards. You’ll feel more excited about achieving your goals because they’re specific and measurable. If you have clear goals, there’s a way for you to measure whether or not they’ve been achieved.
What Are SMART Goals?
SMART goals are specific, measurable, achievable, relevant, and time-bound. They’re also relatively easy to remember as you write them down.
Select A Goal Tracker
Now that you have your goal, it’s time to pick a tracker. You want one that is easy to use, compatible with your phone and computer, and free (the first two are more important than the latter). We recommend using SMART Goal Tracker, available on Android and Apple platforms. It works like this: every day, you log into the app, set a weight loss goal for yourself based on the numbers above (for example: “I want to lose 2 pounds per week”), then each time you weigh yourself in at least once per week or so (preferably daily), enter in how much weight was lost since last time. You’ll get an alert when you’ve reached your goal!
Create A Dedicated Time For Tracking Your Weight Loss Goals
You may already be tracking your progress somehow, but if not, it’s important to do so. The key is consistency. The more consistent you are with monitoring your weight loss goals, the better your chance of achieving them.
It can be tempting to weigh yourself once a week and call that good enough—but this method is far from ideal. If you’re going to make real progress toward your goal, then tracking it daily or even multiple times per day is necessary. What’s more, weighing yourself daily will help keep you in check when trying to lose weight because it provides a sense of empowerment instead of discouragement when looking at the scale go up or down on any day (which happens).
Have An Flexible Approach
You should have a flexible approach to your goals. This is because you might change your mind even if you have set the most realistic and achievable weight loss goals. Therefore, it is best to be open-minded and flexible regarding this process. Always remember that there are no rules when it comes to weight loss.
Also, avoid getting too attached to your goal because this could worsen things if they don’t happen as planned or expected. For example, if you want to lose 20 but lose only 10 pounds in two months, then don’t get upset because nothing went wrong!
Let’s say that after two months (or a month), things changed such that now we need more time for us (our body) to achieve our final goal, which is losing 20 pounds; well then maybe our first goal was unrealistic or just too short of a timeframe so we should work on changing our current situation into something better – maybe increase our efforts or focus more on other areas which will help us achieve our new goal (which may be higher than what we previously wanted).
Logging Daily Food & Drink Intake For Every Next Week

The key to successfully logging your food & drink intake is to ensure you’re honest about what you’ve eaten and drank. Logging daily food & drink intake is so important we recommend that you dedicate at least 15 minutes each day to logging what you’ve eaten and drank for the next week (i.e., for seven days). It’s important to know exactly how much sugar, fat, and salt are in each meal so that you can properly adjust your goals for next week based on what happened this week (as well as any other factors).
If you’re unsure what to eat and drink, it’s best to consult a nutritionist who can help you create meal plans based on your goals. This is especially important if you want to lose weight or gain muscle. Consider hiring a personal trainer who can show you how to properly perform exercises that will help with weight loss/gain (e.g., strength training versus cardio).
Drink 64 Ounces Of Water Each Day For Next Week

Water is one of the most important things for your body. It helps flush out toxins from your body and keeps you feeling full, so you don’t overeat. To reach your weight loss goals, you must drink enough water.
The Institute of Medicine recommends that adult women consume about 91 ounces of total beverages daily (including water), while men should consume about 125 ounces daily. You can achieve this goal by drinking one glass of water after each meal and snack and drinking other beverages if desired.
The key is filling up on liquid and ensuring it’s clean and healthy! That means no sugary drinks like soda or fruit juice – these will only lead toward weight gain because they’re filled with empty calories and sugar that won’t fill anyone up but rather leave them craving more food later down the road after their blood sugar spikes then crash again soon after that.”
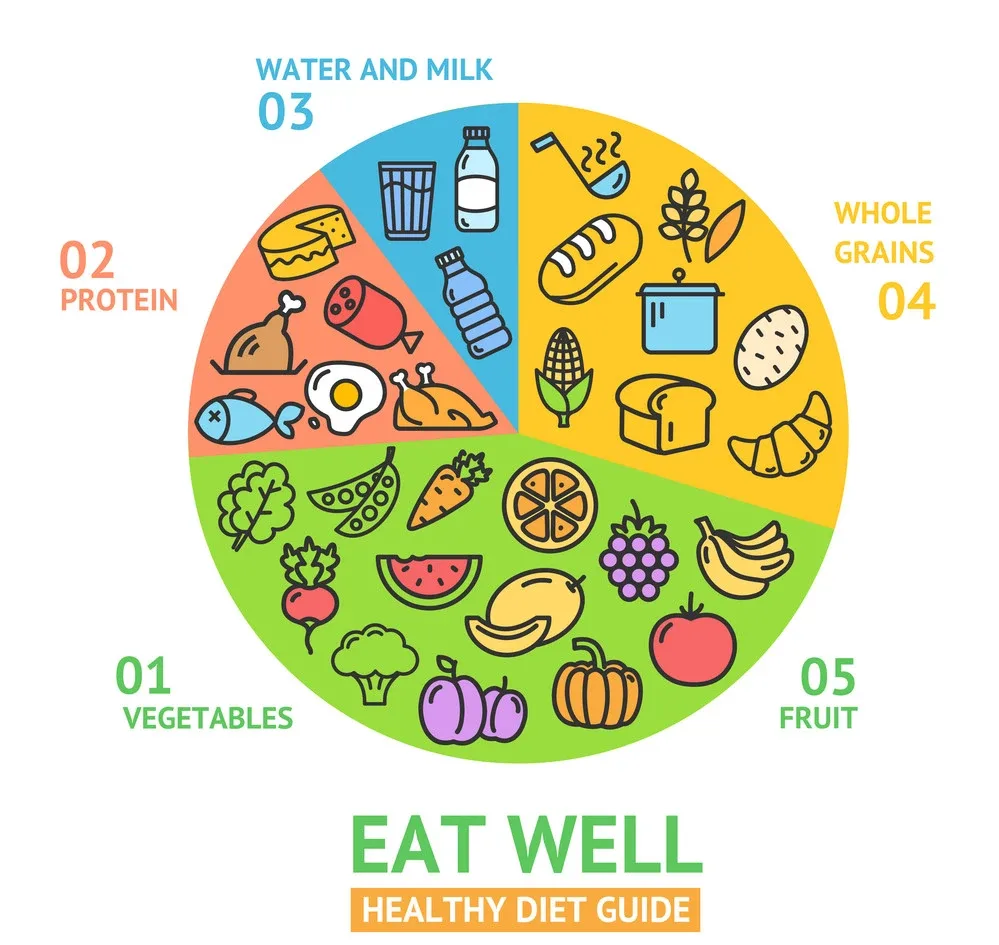
Add Non-Starchy Vegetables To Two Meals Per Day Daily For Next Week

Add non-starchy vegetables to two meals per day for the next week. Non-starch vegetables are a great way to increase your daily vegetable intake.
From cauliflower, cabbage, and celery to green beans, kale, and lettuce, there are all kinds of options that don’t have any starch or sugar in them, so you can enjoy the benefits without worrying about adding too many carbs to your diet.
Increasing Your Step Count For Week By 1,000 Steps Per Day
You’re looking to increase your step count for the week. Add 1,000 steps per day to your current average and see if you can keep it up. If so, great—you’ll be on your way to at least 10,000 steps per day!
I have a couple of suggestions that will help you get there:
- Walk to work or school instead of driving. You may have to do this in shifts, so you’re not stranded without a car during bad weather or emergencies. Swapping out one of your car trips for a walk is an easy way to add several thousand steps into your routine each week.
- Use a fitness tracker to track how many calories you burn daily and ensure you hit at least 10,000 steps daily!
Conclusion
It’s important to remember that weight loss goals can be challenging to achieve and even harder to maintain. That said, following our advice will help you set realistic goals for yourself, motivating you throughout the process.