
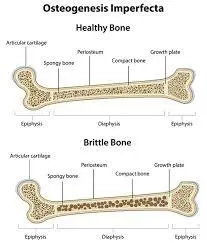
Osteogenesis imperfecta (OI) is a genetic condition that causes bones to break easily. It results from a mutation in the COL1A1 gene, which makes collagen, the protein that gives bones strength and flexibility. The disease is inherited in an autosomal dominant pattern: If one parent has OI, there’s a 50 percent chance each child will inherit it. The symptoms of OI vary significantly in severity among affected individuals within families, even among siblings with the same mutation.
What are the types of osteogenesis imperfecta?
Osteogenesis imperfecta can be divided into two main types:
- Type I, or classic OI
This is the most common disorder characterized by normal bone density (as seen on x-rays) with soft, flexible bones that break easily. While it’s possible to have this type with any skin color, people with classic OI are often blue-eyed blondes because their genes determine the eye and hair color.
- Type II, or brittle bone disease
This less common osteogenesis imperfecta is usually more severe than type I. The bones tend to fracture easily, even without trauma or impact, typically forming thin plates rather than being strong and pliable like healthy bones. This is also known as “brittle bone disease” because fractures occur due to small amounts of pressure instead of one large blow, as in classic OI patients.
What are the symptoms of osteogenesis imperfecta?
- Bone fragility
- Loss of height
- Dental problems, including malocclusion (misalignment of the teeth) and tooth fractures
- Slowed growth
- Osteoporosis causes bones to break more easily. If your child has osteogenesis imperfecta, they will likely develop osteoporosis as an adult.
How is osteogenesis imperfecta (OI) diagnosed?
Osteogenesis imperfecta is usually diagnosed by a doctor. The doctor will start with a physical examination, which includes looking at your child’s bones and joints. Your child’s doctor may also order blood tests to see if they have other medical problems.
The diagnosis of osteogenesis imperfecta is made by looking at your child’s bone x-rays, which show how the bones are shaped and whether they are weak or fractured. It can be hard to tell the difference between milder forms of OI and other conditions that cause weak bones or fractures, such as rheumatoid arthritis or scoliosis (curvature of the spine).
How is osteogenesis imperfecta (OI) treated?
The treatment for osteogenesis imperfecta (OI) depends on how severe the disease is and whether it’s mild, moderate, or severe.
- Fracture Care

If you have OI, it is important to maintain good bone health and avoid fractures. Maintaining strong bones is the best way to prevent bones from breaking during daily activities or sports. Talk with your doctor about the right activity based on your condition.
Most people with OI will be able to do most things if they take proper precautions, such as participating in potentially dangerous activities. As you age, it may become more difficult to manage your condition because of its impact on bones; however, many medications and treatments available can help.
- Physical Therapy

Physical therapy for osteogenesis imperfecta is a way to rehabilitate the body and improve mobility and strength. Physical therapists can help with joint pain, muscle weakness, balance, posture, and breathing. They can also help people with OI speak clearly and improve their range of motion in the throat so they can eat and drink more easily.
Physical therapists use different treatment methods, including:
-Exercise
-Balance training
-Weight-bearing activities (such as walking)
-Stretching exercises (like yoga)
- Bracing

Bracing can prevent fractures, treat fractures and manage pain and other symptoms. It should be worn for as long as possible, but children may not need to wear the brace throughout their entire lives. Braces help prevent spine deformities and back pain in people with OI.
Bracing is usually most effective when it’s started early in life because this will allow your child’s bones to grow stronger over time. Bracing also helps with mobility so that you can move around easier and play sports without worrying about breaking a bone.
- Surgical Procedures

Several surgical procedures help treat Osteogenesis Imperfecta. They include:
- Osteotomies are small cuts in the bone, which are made to relieve pressure on the spinal column and separate fused bones.
- Fusion is a procedure where two or more vertebrae (the bones in your spine) have been joined together by a fusion device (such as an expandable rod).
- Grafting is when a graft fills areas of weakened bone caused by fractures. This can include synthetic materials like those used for other implants or natural materials. These grafts usually grow over time into more solid structures than those created with synthetic implants.
- Interbody bone grafting involves removing some discs from between vertebrae using special instruments designed specifically for this purpose; then filling in their place with either traditional interbody spacers made out of metal alloys or newer plastic devices called “ceramic interbody spacers” (C-spacers). Both types work well at relieving pain and reducing stress on nearby nerves while helping prevent further deterioration toward spinal collapse conditions such as scoliosis without needing additional surgery down the road!
- Medication

Your doctor may recommend medications to help manage your symptoms.
Anti-inflammatory drugs and painkillers can alleviate pain caused by breaks in the bones. Calcium and vitamin D supplements are sometimes recommended to keep your bones strong.
Conclusion
Osteogenesis imperfecta is a rare genetic disorder that affects the bones and joints. It can cause painful fractures, muscle weakness, and other complications that make life difficult for those affected by this condition. The treatment options vary depending on the severity of symptoms and how they impact daily life.



[…] Do you know What is the treatment for Osteogenesis Imperfecta? […]