Does polycystic ovary syndrome cause diabetes?
Houston Endocrine Center2022-11-23T14:57:23+00:00
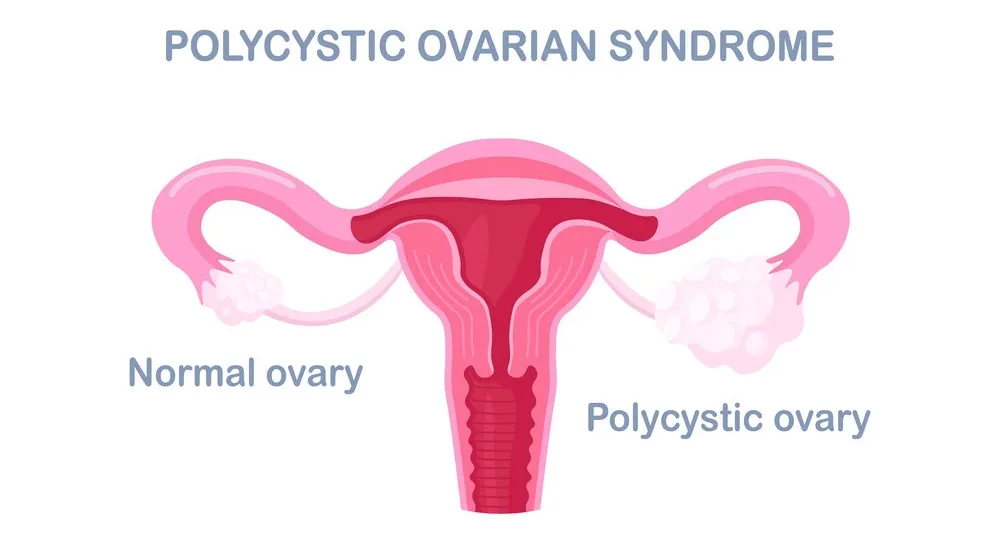
Polycystic ovary syndrome (PCOS) is when a woman has excess male hormones and cysts in her ovaries. It can cause irregular periods, infertility, weight gain, and acne. If you have PCOS, your chances of getting pregnant without medical intervention are only about 25%. That’s why many women with PCOS want to know: Does polycystic ovary syndrome cause diabetes? Well… maybe! Let’s break things down:
Polycystic ovary syndrome (PCOS) has been linked to diabetes.

Polycystic ovary syndrome (PCOS) is a condition that affects the reproductive system. It’s a common cause of infertility and can be associated with an increased risk of developing type-2 diabetes. In women with PCOS, excess male hormones can affect their menstrual cycle. This can lead to changes in ovulation and other problems with fertility.
The symptoms of PCOS vary widely from woman to woman and may not show up until someone becomes sexually active or goes through menopause. In some cases, it’s possible for people who don’t have any signs or symptoms not even realize that they have this condition until they’re diagnosed during pregnancy or by their doctor after giving birth.
How does PCOS relate to diabetes?

If you already have PCOS, you may be at an increased risk of developing this problem because obesity—a risk factor for both PCOS and type 2 diabetes—can cause insulin resistance. Insulin resistance is when your body makes insulin but has difficulty using it effectively. This often leads to type 2 diabetes (a form of diabetes that typically occurs late in life).
How PCOS can lead to prediabetes and diabetes
It is important to note that there are other risk factors for developing diabetes. PCOS is a risk factor, but it is not the only one. Some people with PCOS develop diabetes, while others do not. The exact mechanism of how PCOS leads to diabetes is unclear, and the relationship between PCOS and diabetes is complex.
There are two types of diabetes: type 1 and type 2 (you may also hear these referred to as insulin-dependent or non-insulin-dependent). With type 1 diabetes, your pancreas no longer makes insulin—a hormone that allows your body’s cells to use blood sugar for energy—so you will need daily injections of synthetic human insulin for your body’s cells to use blood sugar properly. Type 2 diabetes accounts for 90% – 95% of all diagnosed cases worldwide and occurs when the pancreas does not produce enough insulin and body tissues become resistant to its effects.
PCOS and gestational diabetes
PCOS is a risk factor for gestational diabetes, so it’s important to manage PCOS if you’re pregnant. Managing your symptoms of PCOS will help prevent the development of gestational diabetes. If you have PCOS and are planning to be pregnant, talk to your doctor about ways to prevent gestational diabetes.
If you have PCOS and develop gestational diabetes during pregnancy, managing your symptoms will help lower the risk that complications will occur in the future.
What About Other Types of Diabetes?
But what about other types of diabetes? It’s well known that PCOS is associated with type 2 diabetes, and insulin resistance may influence both conditions. Women with PCOS have nearly double the risk of developing type-2 diabetes compared to women without PCOS.
Other research has also shown that women who have been diagnosed with gestational diabetes or prediabetes during pregnancy are more likely than other pregnant women to develop PCOS afterward.
This suggests that these states have something in common—we now know it might be insulin resistance. But this wasn’t always the case; it was only recently that researchers began looking at how insulin resistance could play a role in PCOS development and progression toward metabolic syndrome (a collection of symptoms associated with increased risk for heart disease).
What does the research say about PCOS’s link with diabetes?

The evidence is clear: PCOS is associated with an increased risk of diabetes.
A 2011 study found that women with polycystic ovary syndrome have higher levels of insulin resistance and are more likely to develop type 2 diabetes than women without the condition. Having PCOS increases the risk of type 2 diabetes by 80%. In another study that followed over 4,000 women for 20 years, researchers found that those with PCOS were twice as likely to develop insulin resistance compared to their peers without it. This suggests that if you have PCOS, you are more likely than other people to develop prediabetes or type 2 diabetes later in life—but not necessarily right now!
A 2015 study published in Diabetes Care also found an association between increased fasting blood sugar levels and hirsutism (excess hair growth on the face) among women with the polycystic ovarian syndrome.* While this relationship doesn’t prove causation (it could be that both conditions share some common cause), it does suggest a connection between them.*
Women with PCOS are more likely to have insulin resistance, which can lead to diabetes.
A woman with PCOS may have insulin resistance, which means her cells aren’t responding efficiently to the hormone insulin. Insulin helps the body’s cells absorb glucose from the bloodstream so it can be used for energy by tissues and organs. When your cells don’t respond well to insulin, your pancreas has to make more of it and secrete it into your bloodstream, which leads to high blood sugar levels over time.
If you’re diagnosed with PCOS, talk with your doctor about getting screened for diabetes so you can get treatment as soon as possible.
Conclusion
So, what does this mean for you? If you have PCOS, it’s important to be aware that your risk of developing diabetes is higher than average. And if you are pre-diabetic or diabetic, you must talk to your doctor about treating the underlying cause of your condition—PCOS—before focusing on managing the symptoms.
