If you’re not getting enough calcium in your diet or have a condition that interferes with how your body absorbs or uses calcium, you may be at risk of osteoporosis. This condition causes bones to become weak and brittle, increasing the risk of fractures and other injuries. The great news is that you can do so many things individually and with your doctor to increase bone density.

This article will discuss improving your bone health through diet and helping prevent bone loss and fractures.
1. Weightlifting and strength training

You can increase your bone density by building muscle. Muscle is denser than fat, so it’s a great way to get extra bone support without resorting to supplements or surgery. If you last exercised a while ago and are worried about how much weightlifting you need to do, don’t be! Most experts recommend two 15-minute weekly strength training sessions targeting all your major muscles (legs and glutes, chest and back).
If you’re looking for something with less impact on your joints but still provides resistance for building muscle, consider yoga or pilates. These classes will improve flexibility and help build balance and coordination—all things that help support healthy bones.
Yoga poses like a downward dog (to strengthen hamstrings) and cat-cow (to stretch hips) can work wonders for improving posture too!
If you’re worried about putting on weight, don’t be! Even if you don’t lose pounds, strength training can help prevent weight gain. That’s because the more muscle mass you have in your body, the more calories you burn throughout the day. It’s a win-win situation!
2. Eating more vegetables

There are many reasons why eating more vegetables is good for your bones.
Vegetables contain vitamins, minerals, and fiber that help your body absorb calcium better. They also make you feel full longer, so you won’t be so hungry when it’s time to eat again.
Vegetables come in a wide variety of shapes, sizes, and colors. Ensure you eat many different kinds daily to get all the necessary nutrients! You can eat them raw or cooked (steamed or boiled) and add them to soups, stews, casseroles, and stir-fries.
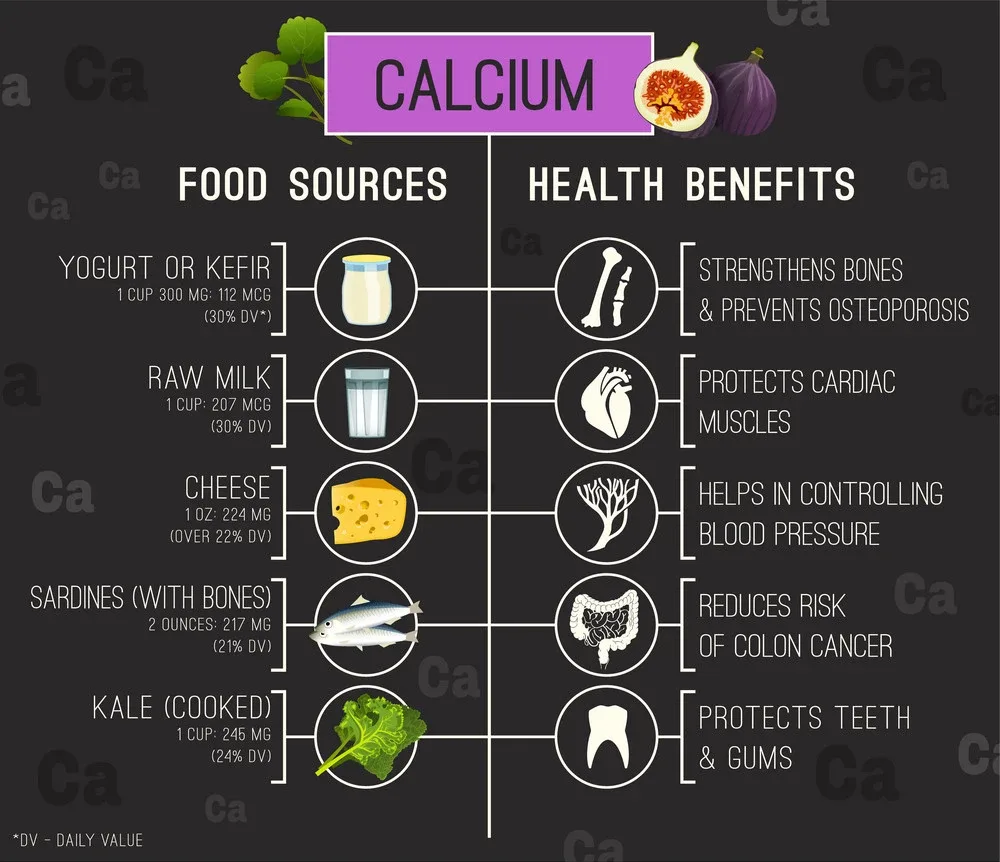
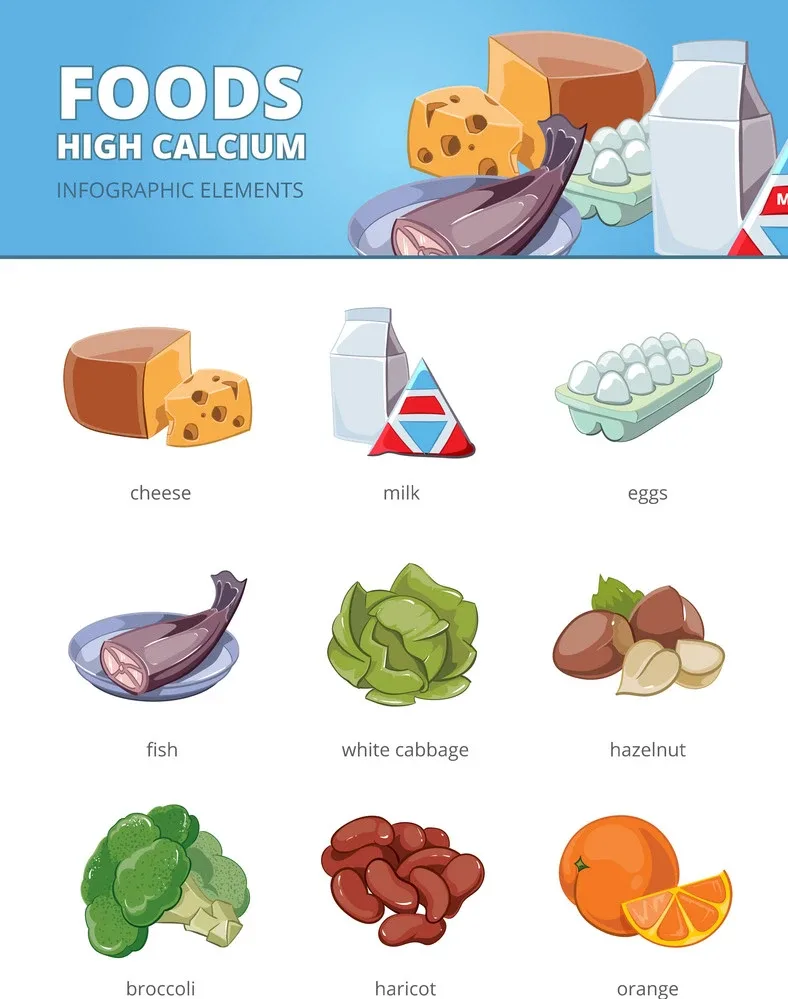
3. Consuming calcium throughout the day

You can increase your bone density by consuming calcium throughout the day. Calcium is found in dairy products, green leafy vegetables, nuts, and seeds. The recommended daily intake of 1,000 milligrams is easily achieved with three servings of low-fat dairy products per day or by eating various foods that contain calcium daily. Another way to get calcium is by adding it to your diet through fortified foods such as breakfast cereals and orange juice.
4. Foods rich in vitamins D and K

Some nutrients are important for building healthy bones. Vitamin D helps your body absorb calcium, which is found in fish, eggs, and fortified milk. Vitamin K is found in leafy greens and other vegetables like broccoli. Another nutrient called magnesium helps your bones stay strong by supporting the production of collagen, which provides a structure for bones and joints. Other foods high in this mineral include spinach, nuts, and seeds.
The best method to get vitamin D is sunlight exposure (up to 15 minutes three times per week). But you must get enough sun exposure daily or live far from the equator (where there’s less ultraviolet light). In that case, talk to your healthcare provider about taking a supplement or multivitamin with at least 400 IU of vitamin D3 per day—the recommended dietary allowance (RDA) is 600 IU daily for adults between 19–70 years old who aren’t pregnant or breastfeeding; 800 IU after age 70.
5. Maintaining a healthy weight.

Weight and bone density are related. Being overweight increases your risk of osteoporosis. You can improve your bone health by maintaining a healthy weight and staying active. A balanced diet rich in calcium, vitamin D, and other nutrients is also important for building strong bones.
The National Osteoporosis Foundation recommends healthy weight goals as follows:
- Women should aim for a body mass index (BMI) between 19 and 25 (depending on height). For example, a woman who measures 5 feet 5 inches tall would want her BMI to range from 104 pounds to 124 pounds; she would be considered underweight if she weighed less than 104 pounds or overweight if she weighed more than 124 pounds at that height.
- Men should aim for a BMI between 21 and 30 (depending on height). For example, a man who measures 6 feet 1 inch tall would want his BMI to range from 126 pounds to 184 pounds; he would be considered underweight if he weighed less than 126 pounds or overweight if he weighed more than 184 pounds at that height.
6. Avoiding a low-calorie diet

A low-calorie diet, typically defined as less than 1,200 calories a day for women or 1,500 calories a day for men, can lead to a loss of bone density. In addition to being problematic for your bones, a low-calorie diet is also not recommended for people older than 65 because it may increase their risk of heart disease and stroke. If you’re 50 years old or older and have osteoporosis or osteopenia (loss of bone mineral density), talk with your doctor before starting any weight loss plan.
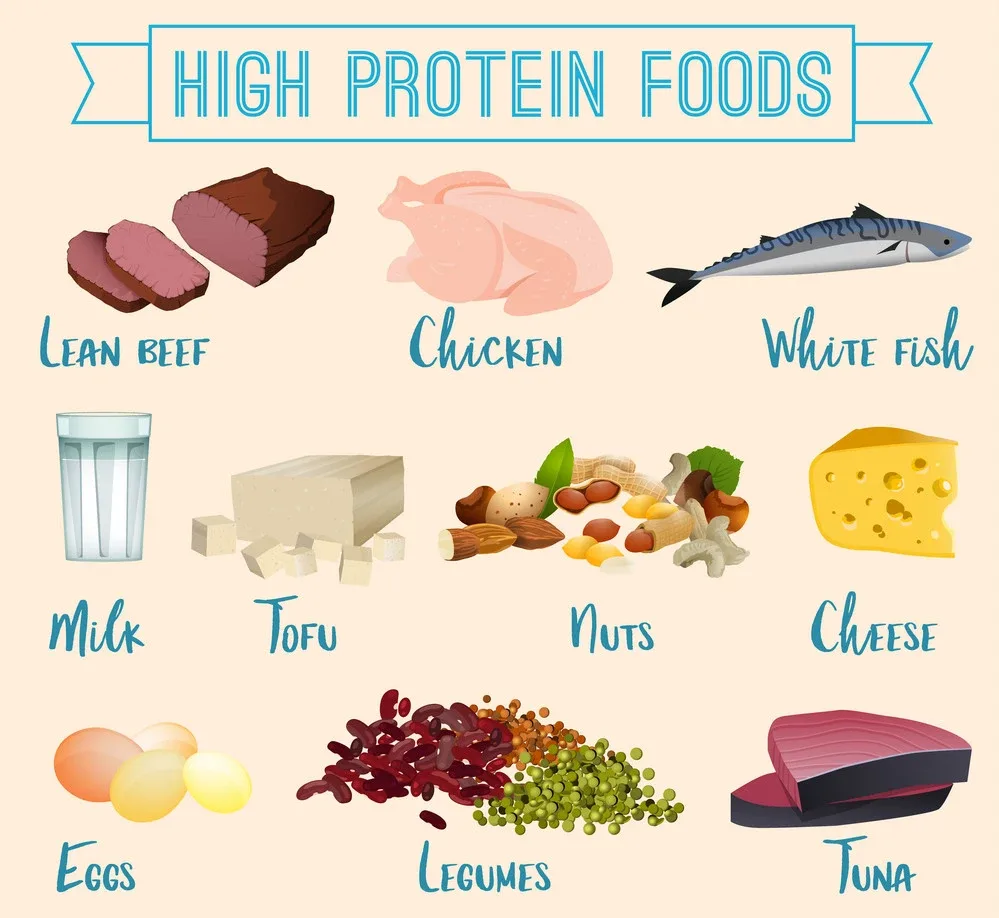
7. Eating more protein
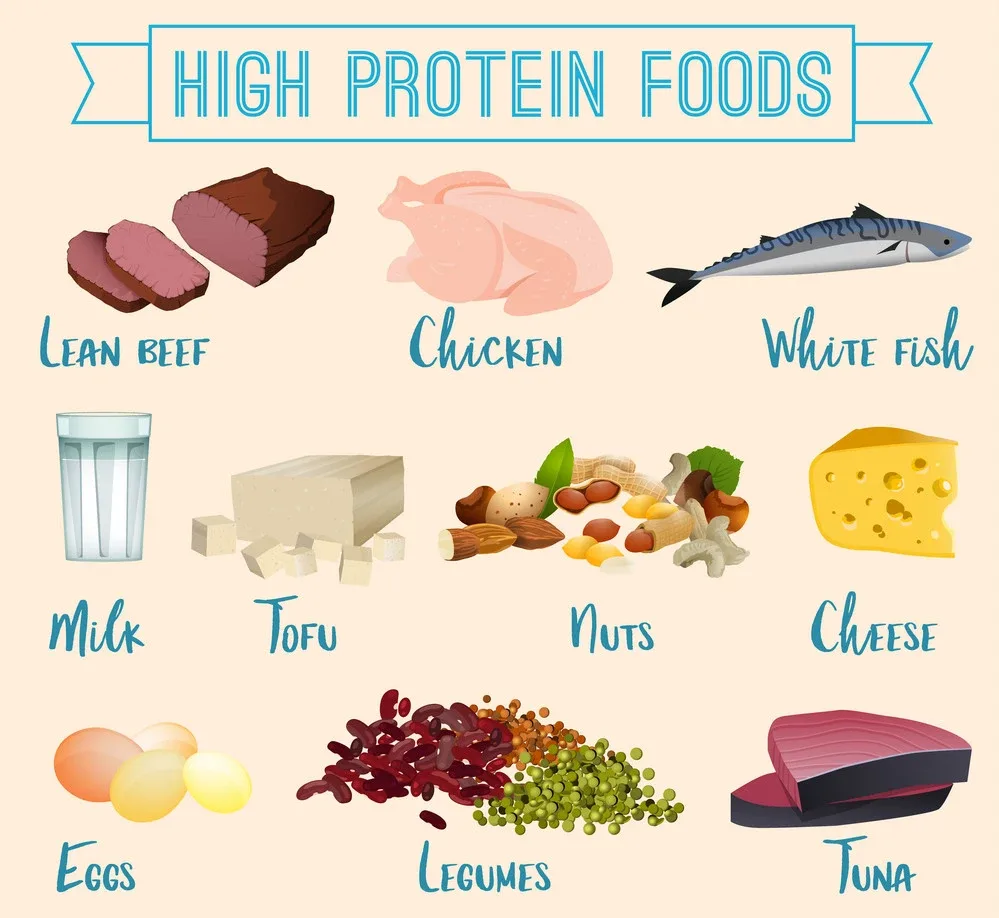
Protein is an essential nutrient that builds and maintains bones. Protein helps keep you full, too, so eating more can help you eat less overall.
Protein can be found in many foods like meat, fish, eggs, and dairy products. Some plant foods (beans, nuts, and seeds) contain protein.
How much daily protein you need depends on your age and gender:
- Children ages 1 to 3 need 13 g of protein per day.
- Men over age 51 should get 56 g of protein per day, while men under 51 should get between 44–56 g of protein per day, depending on their activity level. Women over 51 should aim for 46–56 g of protein per day, while those under 51 should aim for 41–46 g per day, depending on their activity level.
- If you’re pregnant or breastfeeding, you need more than the general recommendations.
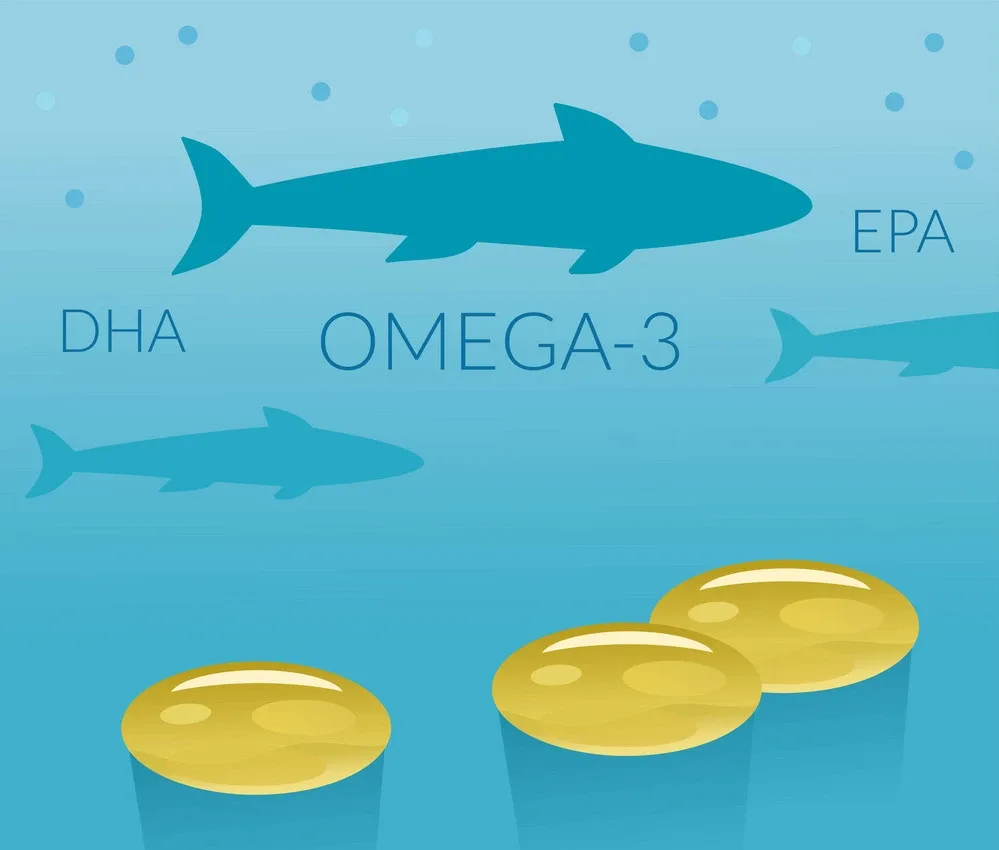
8. Eating foods rich in omega-3 fatty acids
Omega-3 fatty acids are found in fish and nuts and are good for your heart and brain.
Here’s where it gets interesting: Omega 3s can also help increase bone density by reducing inflammation in the body. This is good news because inflammatory processes cause bone loss by increasing bone breakdown while slowing down new bone formation. If you have an inflammatory disease like arthritis or diabetes, adding more omega-3s to your diet may help protect you from losing bone mass due to those conditions.
9. Eating foods rich in magnesium and zinc

Two other nutrients you can increase your intake of are magnesium and zinc.
Magnesium is found in dark leafy greens, nuts and seeds, beans, whole grains, and bananas. It has been shown to contribute to bone health by reducing stress fractures in runners who consume more than 400 mg daily. Zinc is important for red blood cell formation (which transports oxygen throughout the body) and for building muscles that support bone mass. Foods high in zinc include pumpkin seeds, cashews, beef, and pork (particularly when lean cuts are used).
10. Stopping smoking

Smoking has been shown to reduce the amount of calcium in your bones, which can affect their strength and make them more susceptible to fractures. Smoking harms bone density and can increase the risk of osteoporosis. One study found that heavy smokers have as much as 20% lower bone density than nonsmokers.
The best way to quit smoking is by setting a date and sticking to it. The sooner you stop smoking, the less time you’ll spend suffering from its harmful effects on your health—including increasing your chances of developing osteoporosis later in life!
11. Avoiding excessive drinking

If you’re going to drink alcohol, it’s important to remember that this can negatively affect your bones. Alcohol may lead to a vitamin deficiency and a calcium deficiency, which can put you at risk for osteoporosis.
Excessive drinking can also be bad for your health overall. When you drink too much alcohol or binge drink (defined as consuming five or more drinks in one sitting), it increases the risk of chronic diseases like liver disease, heart disease, stroke, and some cancers. In addition to these risks associated with excessive drinking, some behavioral changes are associated with heavy drinking.
Conclusion
If you want to increase your bone density, you can do many things. Exercise and a healthy diet will help increase the amount of calcium in your bones and help your body absorb more calcium from food sources. If you’re concerned about osteoporosis and want to know if it affects your bones, consult your doctor about getting a bone density test.