Why is the pituitary gland known as the master gland?
Houston Endocrine Center2022-12-10T15:02:36+00:00The pituitary gland is the master gland because it controls other bodily glands. It plays a role in reproduction and releasing hormones from other glands (such as the thyroid and adrenal). This means that when something goes wrong with your pituitary gland, it can simultaneously affect many other body systems.

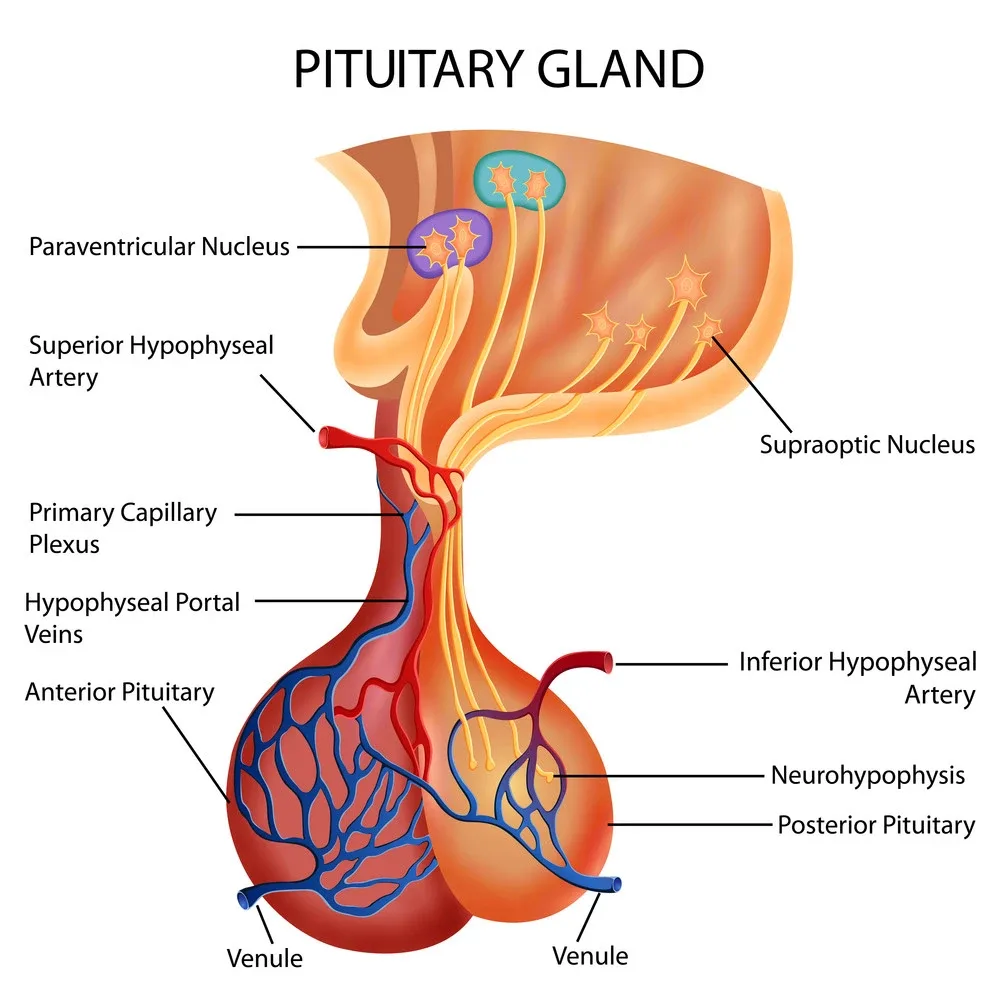
Anatomy of the pituitary gland
The pituitary gland is a small-sized structure connecting your hypothalamus and the brain stem. It produces hormones that control growth, metabolism, thyroid function, and sexual development. The anterior lobe of the pituitary gland makes up about 80% of its volume and produces six hormones:
- Luteinizing hormone (LH)
- Adrenocorticotropic hormone (ACTH)
- Growth hormone (GH)
- Thyroid-stimulating hormone (TSH)
- Prolactin (PRL)
Can you live without a pituitary gland?
The pituitary gland is essential to life. It’s the master gland, and without it, you would die.
The pituitary gland is located in the brain’s center behind your nose. The size of a pea makes many hormones that control other glands in your body. These include your thyroid and adrenal glands (which make stress hormones).
These hormones help manage growth, appetite, and moods such as depression or mania. They also affect sexual development during puberty, pregnancy, and breastfeeding after having children.
The function of the pituitary gland
The pituitary gland produces hormones that control other endocrine glands (a group of cells that produce chemicals used for communication between cells). For example, one type of hormone produced by the pituitary tells your thyroid to produce more or less thyroid hormone; another type tells your adrenal glands to produce more or less adrenaline; yet another controls growth and sex hormones.
The pituitary gland is made up of multiple lobes, which are separated by fluid-filled spaces. The most important parts of the pituitary gland are called the pars distalis or anterior lobe. This part produces growth hormone (GH), prolactin, and melanocyte-stimulating hormone (MSH).
GH is responsible for increasing the size of your muscles and bones, while MSH helps regulate the production of melanin (the pigment which gives skin its color). Prolactin is a hormone involved in lactation.
The pituitary gland and its hormones are important for several reasons. For example, if you have too much MSH in your body, you may experience hyperpigmentation (a darkening of the skin) or melanoma (skin cancer caused by excessive exposure to sunlight). Similarly, too much prolactin can cause lactation (breast milk production), which is why breastfeeding mothers produce more milk than other women.
The pituitary gland is also responsible for controlling the production of sex hormones. These hormones, such as testosterone and estrogen, are responsible for sexual development in both men and women. For example, testosterone has several functions in males, including increasing muscle mass, promoting hair growth on the face and body, and determining sperm production. Estrogen plays an important role in fetal development by producing male sex characteristics like testicles (testes).
Where is the pituitary gland located?
This gland is located in the brain. It’s positioned between the front of your nose and forehead, right above your nasal passages. The gland is also known as a pea-sized lump of tissue because it looks like a small pea when you look at it through an endoscope or microscope.
The pituitary gland is part of an important structure called the hypothalamus, which regulates many functions in your body, including reproduction and growth hormone production. The pituitary connects to other parts of your body through a network of blood vessels that carry hormones to other organs where they work their jobs (see “Hormone Production”).
Conclusion
The pituitary gland is one of the most important glands in your body. It is responsible for producing many hormones, including oxytocin and growth hormone. This article has explained how it works and why it’s called the master gland.