Osteoporosis is a disease that causes the bones to become brittle and weak. Osteoporosis can lead to fractures in the hip, spine, or wrist. You may have heard that osteoporosis affects only older people, but 10 million Americans under 50 have the disease. It’s normal to have questions about this common bone disease, but don’t worry! This blog will answer all of your questions about what osteoporosis is and does osteoporosis affect your teeth.

What are teeth made of?
Your teeth are made up of three tissues:
- Enamel, the hardest substance in your body, covers the crown of each tooth. It helps prevent cavities and tooth decay.
- Dentin is a hard but flexible tissue that makes up most of the tooth except for its outer layer (enamel).
- Pulp is a soft tissue that contains nerves, blood vessels, and connective tissue. It’s found inside the root of your tooth and connects it to your jawbone.
What Is the Connection Between Osteoporosis and Oral Health?
Osteoporosis can affect your oral health in several ways.
- Tooth loss: Bone loss can lead to tooth loss, which can cause eating and chewing difficulties. If you’re losing bone faster than it’s being replaced by new bone (which happens as you age), your teeth may become loose and fall out. This is called “tooth resorption.”

- Gum disease: As osteoporosis progresses and the bones become weaker, they can’t protect the gums from infection anymore, making it easier for bacteria to enter the body through the gum tissue around your teeth. The bacteria that cause gum disease thrive when there are gaps between your teeth where food gets stuck or sits too long between brushings; this leads to plaque buildup that eventually causes inflammation in the mouth—a condition known as periodontitis (periodontal disease). Symptoms include swollen gums and bleeding when you brush or floss; bad breath; receding gums that expose more of each tooth surface; a change in bite pattern due to uneven gum line growth patterns; chronic soreness or tenderness of cheek surfaces near either side of the lower front four central incisors (“cheek abrasion”); loose teeth due to shifting positions within sockets as well as deterioration from lack of support from surrounding structures like ligaments holding them upright in place,” says Dr. Niamh O’Reilly at The Bali Dental Clinic who also adds that some people experience no symptoms but still suffer with advanced cases of periodontal disease.”
Research findings

Research findings show that there is a connection between osteoporosis and oral health. The link between the two needs to be better understood, however. Many studies have been conducted to understand this connection, but more research is needed to understand the relationship fully. The relationship between osteoporosis and oral health is not well understood, which leaves researchers with many unanswered questions to be answered.
Limiting the Damage
You can do these things to reduce the damage caused by osteoporosis.
- If there’s one thing that will help prevent cavities and gum disease, it’s flossing! Use a soft-bristled toothbrush. A harder brush can wear down your enamel and make it more prone to fracturing when exposed to acids produced by bacteria in your mouth.
- Floss daily if you still need to, or get started if you haven’t been doing it for long.
- Brush your tongue regularly—it helps keep bad breath at bay, too!
- Use mouthwash after meals (especially acidic ones) and before bedtime so as not to disturb the pH levels in your mouth while sleeping—another way of worsening tooth decay over time due to increased exposure times between meals/snacks rather than during meal times alone where most people tend towards snacking anyways.”
Keep Regularly Scheduled Dental Appointments

It’s important to keep regularly scheduled dental appointments. The dentist can help you develop a routine cleaning schedule and identify any problems before they become serious. If you’re unsure where to begin, a dental check-up every six months is an excellent starting point.
If you suspect that your teeth are affected by osteoporosis, the dentist can recommend a suitable course of action for maintaining healthy teeth and gums. They may also offer advice on diet and lifestyle choices that will reduce the risk of tooth decay or other dental issues.
Eat a Healthy Diet
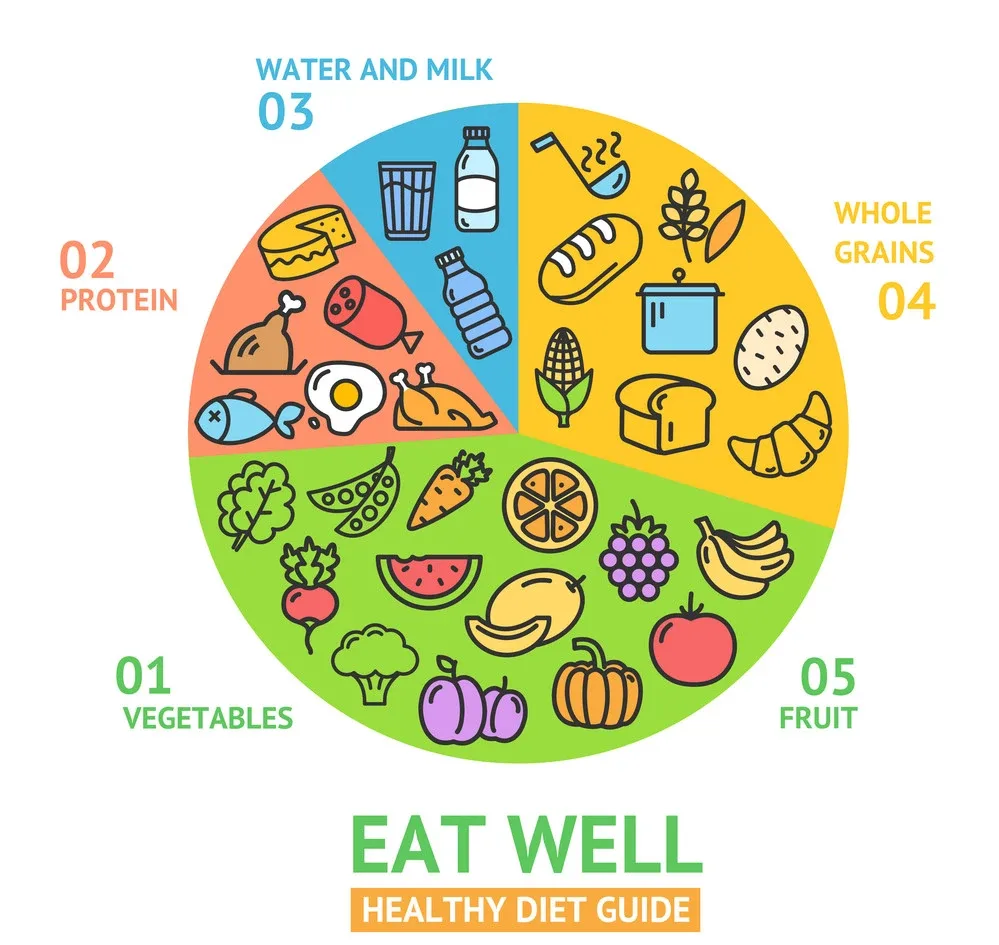
- Eat fruits and vegetables: They are the source of vitamins, minerals, and fiber that help protect your body from disease. They also contain powerful antioxidants that can help slow the aging process.
- Avoid sugary drinks: Sugary drinks like soda and fruit juice have no nutritional value and contribute to tooth decay and obesity. A better alternative is to drink water or low-calorie flavored water (flavored with natural ingredients).
- Eat calcium-rich foods: Calcium helps create strong bones, so people with osteoporosis need to get enough calcium from their diet (especially if they do not take supplements). The sources of calcium include dairy products such as milk, cheese, or yogurt; dark green leafy vegetables such as sardines; almonds; beans; tofu processed with calcium sulfate; salmon canned with edible bone fragments still attached (gives more than 100 mg per 3 oz serving).
Exercise
- Exercise helps your body absorb calcium.
- Exercise helps maintain bone density.
- Exercise helps with weight loss.
- Exercise helps you relax.
Quit Smoking

If you smoke, it’s important to quit. Smoking is a risk factor for oral cancer and can lead to gum disease. In addition, smoking causes bad breath and tooth discoloration. Smoking may also make your teeth more susceptible to decay.
Stop Drinking Alcohol
If you’re drinking alcohol, it’s important to be aware of the following:
- Alcohol can cause tooth decay. When sugar is in your mouth, bacteria feed on it, creating acid that attacks your teeth. This can lead to cavities and other problems, such as gingivitis (inflammation of the gums).
- Alcohol increases the risk of oral cancer. Drinking too much alcohol can cause a dry mouth, which makes you more susceptible to infections like bad breath or periodontal disease because saliva helps wash away bacteria that cause these conditions. People who drink heavily are also more likely to develop other health issues like liver disease or heart disease, which may also result in a dry mouth.
- Suppose you have gum disease, receding gums from an injury, or poor dental hygiene. In that case, drinking will worsen those symptoms by increasing inflammation throughout your body and worsening bone resorption (the process by which old bone cells break down), in addition to accelerating tooth loss due to decay or erosion caused by endodontic therapy (root canal treatment).
Conclusion
We hope this article provides information on the relationship between osteoporosis and oral health. It is important to know that oral health problems are not always caused directly by osteoporosis but can be exacerbated by it. Take care of your teeth so they will last a lifetime!



Leave A Comment