Type 1 diabetes is a very complex disease, and many factors can contribute to the condition. One thing that can be beneficial to the treatment is an insulin pump. A pump sends a continuous supply of insulin with infrequent or no pulses, gradually lowering blood sugar levels without frequent injections.
The benefits of an insulin pump include:
- Stability
- Accuracy
- Convenience
- Lack of the risk associated with hypoglycemia
But what are the unseen benefits of insulin pumps in type 1 diabetes management? Curious to know about them? Read this blog till the end to find out!
What Is Insulin Pump
Insulin pumps are medical devices that deliver insulin to the body. They are used to help control blood sugar levels in people with diabetes or to help them lose weight.
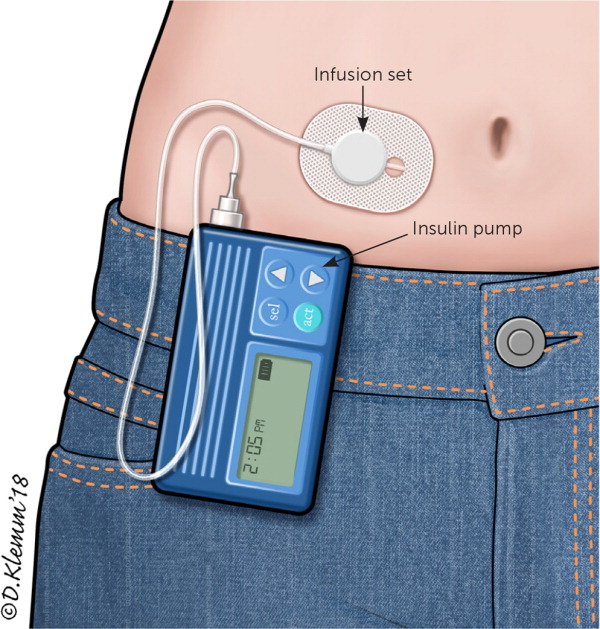
An insulin pump gives users a slower, continuous flow of insulin through a thin tube. Most pumps use a reservoir attached to the body filled with liquid and then pumped up through a needle inserted in the skin near the outer side of the thigh. Some pumps use an infusion set inserted into one of the veins in the arm. Both are medical devices that deliver insulin to the body.

Source: American Nurse
Insulin pumps are important for people with diabetes because they help them manage their condition and prevent complications such as kidney disease, blindness, and amputations. There are various types of insulin pumps. They may be continuous or intermittent and can also be remote or mobile.
They can be used for either long-term or short-term use. A doctor often prescribes an insulin pump to treat diabetes for long-term use. Short-term use means using an insulin pump for less than 90 days.
How Does Insulin Pump Work?
Insulin pumps work by delivering insulin to the body through a tube inserted under the skin in the abdomen or buttocks. The person wears a small device that continuously senses the blood sugar and delivers continuous, variable (on-demand) doses of insulin based on the levels detected.
A person with diabetes has to monitor their blood sugar levels and take insulin injections throughout the day. The patient can choose to use an insulin pump or an insulin pen. A person with a pump can control how much and when they inject, but they still need to review their blood glucose levels before and after meals.
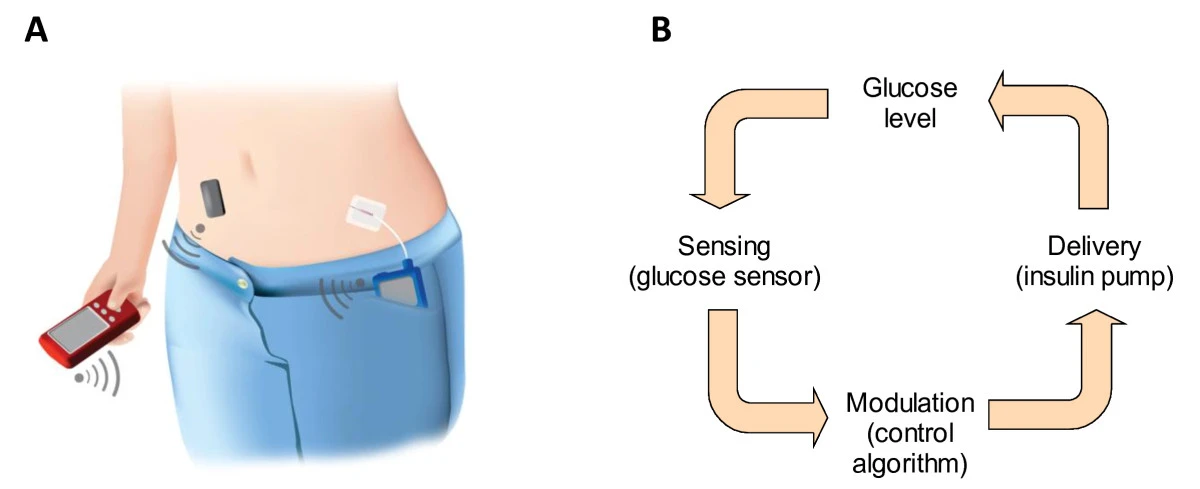
Source: BMC Medicine
Bolus pumps are used to administer fast-acting insulin in response to a meal. Once the pump is activated, it automatically delivers a dose of insulin at regular intervals until the basal rate is reached (usually within 15 minutes) and the pump is turned off. The bolus dose rate can be changed to respond to meal-related blood sugar levels, but a basal rate must be set first. A basal rate sets the amount of insulin delivered per hour, giving a more gradual response to changes in blood sugar levels.
Self-monitoring of blood glucose (SMBG) is an important strategy used by people with type 1 diabetes to decrease the risk for diabetic ketoacidosis, which is a dangerous condition resulting from high blood sugars.
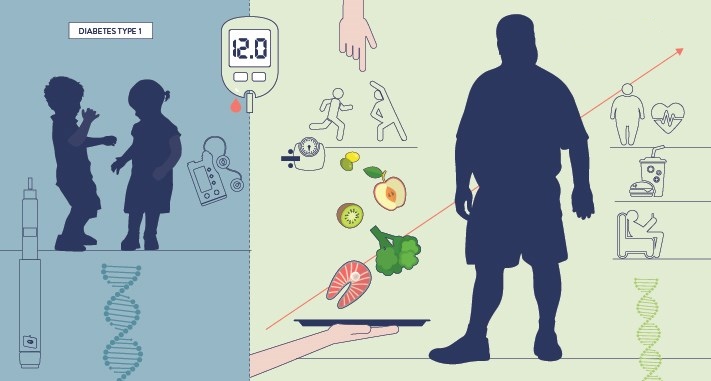
Type 1 Diabetes Management
Type 1 diabetes is a chronic condition where the person’s pancreas stops making insulin, which is required to convert blood sugar into energy.
Type 1 diabetes management is a process that is vital for people with this condition. They need to keep track of their blood sugar levels and keep them as close to normal as possible. This can be done with the help of diet, exercise, medications, and insulin shots.
Managing Type 1 diabetes is a process that includes everything from maintaining blood glucose levels to taking medications and insulin shots. According to the American Diabetes Association, people having Type 1 diabetes must take insulin shots or other medications. These are given to manage their blood sugar levels and maintain a healthy lifestyle.
The 7 Unseen Benefits Of Using An Insulin Pump For Type 1 Diabetes Management
Insulin pumps enable people with diabetes to manage their condition by providing a steady and reliable supply of insulin. There are many benefits of using an insulin pump for type 1 diabetes management. However, many people do not realize the many benefits of using it.
Source: NIPH
Here are 7 unseen benefits of using an insulin pump for type 1 diabetes management:
- Insulin pumps are small and discreet. It is not too bulky like a syringe, and it is easy to carry around in your pocket or bag.
- Insulin pumps allow you to make adjustments on the go without waiting for a doctor’s appointment.
- The insulin pump helps you get the right amount of insulin at the right time, which is essential for managing your blood sugar levels well.
- You can wear an insulin pump 24/7 without worrying about wearing out or damaging it because it doesn’t require any batteries or external power sources.
- If you are physically active, the insulin pump will tell you when your rate of insulin is too high or low.
- If a doctor states that your body can no longer produce enough insulin, it is possible to use an insulin pump as a substitute for injections.
- The pump gives you the option to choose how and when to deliver the right amount of insulin without relying on your body’s natural process.
Insulin Pump Therapy
Insulin pump therapy is a way to deliver insulin through an infusion pump. This means that the pump is used with a needleless plastic tube inserted under the skin in a specific location. The infusion pump delivers insulin through this tube, which travels up to the main body of the device and into the vein or artery to control blood sugar levels.
Insulin pump therapy helps people with diabetes manage their disease. It is a way to control blood sugar levels by delivering insulin through an infusion pump.
Insulin pump therapy has many advantages over other treatment methods like insulin injections and injection pumps. One of the primary benefits is the convenience of this method, which allows for easier management of blood sugar levels and compliance with lifestyle changes.
Insulin pump therapy is commonly used for type 1 and type 2 diabetes. Insulin pump therapy can also be used in patients who cannot use injections or injection pumps due to various reasons such as illness, age, or physical condition.
The following steps are involved in insulin pump therapy:
Step 1
The patient’s blood glucose level is monitored, and an insulin dose is calculated as needed. The pump delivers the calculated amount of insulin from a reservoir located in the device’s body.
Source: American Family Physician
The most commonly used devices are self-contained and portable, which means they only require a small tube inserted under the skin. The tube is connected to a cannula (a small, thin plastic tube) in a reservoir taped to the body below the skin.
Step 2
The patient attaches an insulin pump reservoir (typically containing 100 units of insulin) to the cannula on the abdomen.
Step 3
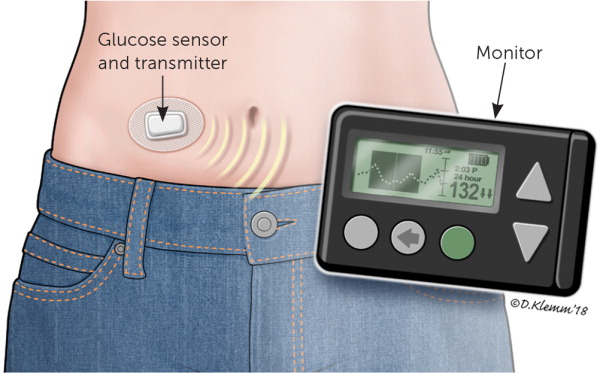
A sensor in the device transmits information wirelessly to the pump and a wireless receiver that displays the glucose information.
Step 4
The device stores up to 1000 units of insulin which can be administered in increments of 0.1 units or 0.25 units.
Step 5
The pump automatically delivers the calculated amount at preset intervals, as needed.
Step 6
The device is programmed with a basal, bolus, or dual-mode to match patients’ needs.
Step 7
The pump displays its current settings, and the last dose is given to know when they are running low on insulin.
Step 8
It has a warning alarm to remind users when their supply is low.
Components Of Insulin Pump Therapy System
The components of the insulin pump therapy system include the pump, infusion set, tubing, and connectors.
Source: American Family Physician
1. Pump
Insulin pumps are used primarily in diabetes mellitus management but can also be utilized for treating hypoglycemia or as an alternative to intravenous delivery of insulin. The pump is a battery-operated device that continuously pumps insulin. Some pumps may be able to operate for two to four years without needing a replacement.
2. Infusion Set
The infusion set is the device that delivers insulin to the body. There are three types of disposable infusion sets:
-
A Cannula
It is inserted directly into a vein.
-
An Intravenous (IV) Set
It uses a large tube inserted directly into a vein or artery.
-
An Intra-Arterial (IA) Set
It uses a small tube inserted through an artery into a large artery.
Intravenous sets are typically used for rapid blood sugar control or emergencies when only a few minutes are available for infusion. An intra-arterial set is typically used when a longer period of insulin delivery is needed; it allows continuous infusion over days to weeks, depending on the size of the vein.
3. Tubing
The tubing is used with the infusion set to transfer the insulin from the reservoir to the body. There are three types of tubing: soft (5/8″ diameter), medium (3/4″ diameter), and hard (1 1/4″). The type of tubing chosen depends on how much insulin is being infused, which arm or leg of the body it will be delivered to, the patient’s weight and size, and the type of insulin.
4. Connectors
Connectors are used to join the tubing to the infusion set. The connectors are made of plastic or metal and have a threaded end that screws into the tube and a needle-pointed end that pierces the skin. The type of connector employed depends on the patient’s weight and the type of insulin.
How Insulin Pump Therapy Can Improve Health (& Life) For People Who Use It
Insulin pump therapy is a treatment for those with diabetes that has been proven to improve health and life. In the past few years, insulin pumps have increased significantly. The benefits of this treatment are numerous, but it is not always easy to find affordable insurance coverage for them.
The benefits of insulin pump therapy are many. It helps prevent the complications of diabetes, such as:
- Blindness
- Heart disease
- Amputations
It also makes it more effortless for people to maintain their weight and live a more active life.
Insulin pump therapy is usually recommended for people who have type one diabetes, as it helps them lead a better life and live longer than those who don’t have it. It also helps them manage their blood sugar levels more easily.
People having type 1 diabetes must take care of their health to live long and healthy lives. The first step is using an insulin pump to regulate their blood sugar levels and ensure they don’t experience dangerous highs or lows.
How Can A Pump Help People With Diabetes Improve Their Quality Of Life?
Diabetes is a severe health condition that impacts millions of people worldwide. With the help of an insulin pump, people with diabetes can achieve better control over their blood glucose levels and brace a healthy lifestyle.
In a study from the journal Diabetes Care, people with Type I Diabetes who regularly used an insulin pump had better control over blood sugar levels than those who did not. The participants in the study were, on average, two years older and showed more signs of diabetes-related nerve damage than those without an insulin pump.

Source: Diabetes.co.uk
People with diabetes are at risk for many complications and require careful monitoring, which can be challenging due to the frequency of blood sugar levels. The use of an insulin pump helps people with diabetes to manage their condition more effectively by controlling their insulin intake and improving their quality of life.
The impact of an insulin pump on quality of life is significant for people with diabetes. It lets them live a normal life without worrying about frequent blood sugar level fluctuations or other complications resulting from diabetes, such as skin infections or kidney disease.
Conclusion And Takeaway
In this article, we discussed the insulin pump and its benefits. We also looked at how it improves the health and life of diabetic people who use insulin pumps.
The conclusion is that an insulin pump is a great option for those who want to regulate their blood sugar levels on their own and are not looking for a long-term solution. It should be used in conjunction with other treatments and lifestyle changes. But it is not right for everyone.
There is a complication of the insulin pump that is less favorable, which is the cost. The “new” pump can cost as much as $8,000 per year for the first few years. This may be an impossible expense for some people with diabetes who don’t have insurance coverage or savings to cover it. The cost is also why most people use a combination of insulin pump therapy, oral medication, and a glucagon emergency injection kit to manage diabetes.
If you want insulin pump management at a reasonable cost, you must book an appointment with us. We are happy to serve our patients with the best quality services at the best rates.



[…] You should also read 7 Unseen Benefits Of Insulin Pump In Type 1 Diabetes Management […]